In this article, it will be explained all about type 2 diabetes and how to manage it with nutrition. In-depth details about this metabolic condition that affects children and adults in modern times.
What is Diabetes?
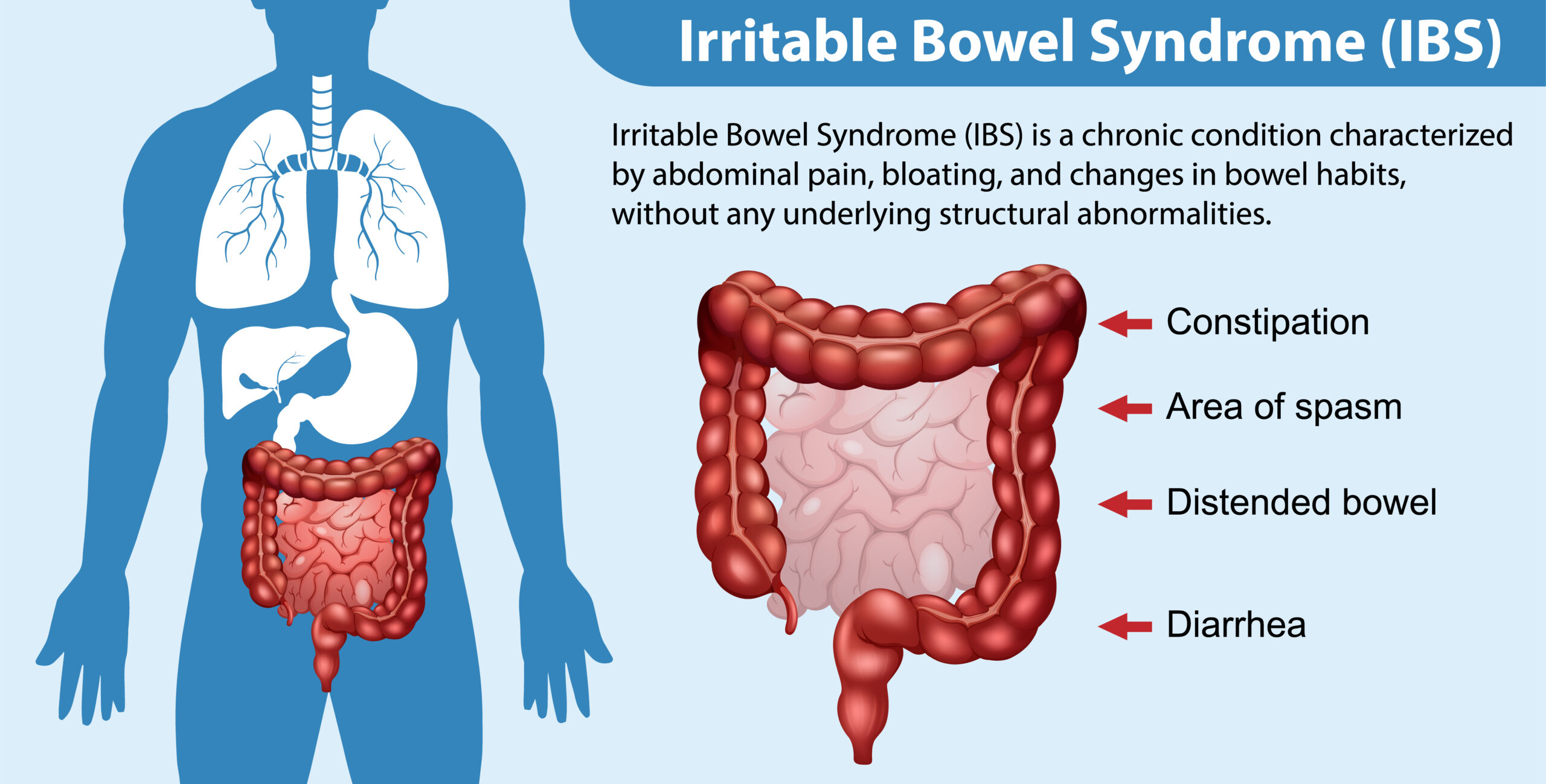
Diabetes is a metabolic disorder characterised by persistent hyperglycemia (high blood sugar levels) due to problems with insulin production or its action. The factors causing diabetes are not yet fully understood, but it is known to have a multifactorial origin, including genetic, biological, and environmental aspects.

Types of Diabetes:
- Type 1A Diabetes: Characterised by autoimmune destruction of pancreatic cells, leading to reduced or, in some cases, complete cessation of insulin production.
- Type 1B Diabetes: Characterised by insulin production deficiency without a known cause.
- Type 2 Diabetes: Characterised by progressive loss of insulin secretion combined with insulin resistance.
- Gestational Diabetes: Characterised by the presence of hyperglycaemia during pregnancy, without a prior diagnosis of diabetes before pregnancy.
- Other less common types of diabetes are monogenic diabetes, and neonatal diabetes, secondary to endocrinopathies, secondary to pancreatic diseases, secondary to infections, and secondary to medications.
90 to 95% of cases are Type 2 Diabetes. In 80-90% of people with Type 2 Diabetes, obesity and metabolic risk factors such as elevated waist circumference, insulin resistance, high blood pressure, and lipid (fat) abnormalities in the blood are associated.
Since Type 2 Diabetes is the most common, let’s go deeper.
Type 2 Diabetes has a strong hereditary component but develops when there is a significant load of environmental factors, such as poor dietary habits and a sedentary lifestyle. It may not present symptoms or may present minimal symptoms for a long period of life, which can lead to rapid progression of its complications.
Therefore, it is important to be aware of risk factors and monitor through exams and medical follow-up.
The main risk factors for the development of Type 2 Diabetes when overweight and obesity are already present include:
- Pre-diabetes
- Family history of diabetes (first-degree relative)
- Women with a previous diagnosis of gestational diabetes
- History of cardiovascular disease
- High blood pressure
- Low HDL cholesterol and elevated triglycerides
- Polycystic ovary syndrome
- Sedentary lifestyle
As mentioned, insulin resistance plays a crucial role in the development of Type 2 Diabetes. But what is insulin resistance?
Insulin resistance consists of a disturbance in insulin signalling, where normal production might occur, but the body responds subnormally to it.
In other words, target tissues are not responding to the hormonal stimulus of insulin due to the desensitization of receptors in these target tissues.
As a result, there is intense stimulation of pancreatic cells to produce more insulin since the tissues are not effectively recognizing the circulating insulin, leading to pancreatic overload, which can eventually result in reduced insulin production over time. Fat infiltration in cells (obesity) and inflammation are key triggers for causing insulin resistance.
It is also important to highlight that there are hormones with effects opposite to insulin, serving as the body’s normal mechanism for self-regulation, such as cortisol, adrenaline, and glucagon. However, in cases where insulin resistance is present, these hormones further intensify the increase in blood glucose levels. Therefore, it is crucial to manage the massive activation of these hormones, such as in situations of intense stress.
Additionally, it is important to mention “skinny fat” individuals, who are metabolically obese, with increased fat tissue in the liver and muscle, inflammation in adipose tissue, reduced muscle mass, and low cardiorespiratory fitness.
Elevated fasting insulin or blood glucose levels suggest insulin resistance. The HOMA-IR test estimates insulin resistance in tissues, while the HOMA-Beta test estimates insulin production in pancreatic cells.
Do you know what the pillars of type 2 diabetes treatment are?
- Healthy eating, both in terms of quality and quantity
- Physical exercise
- Self-monitoring
- Good quality of sleeping
- Knowledge about the disease – self-care

Type 2 diabetes and how to manage it with nutrition
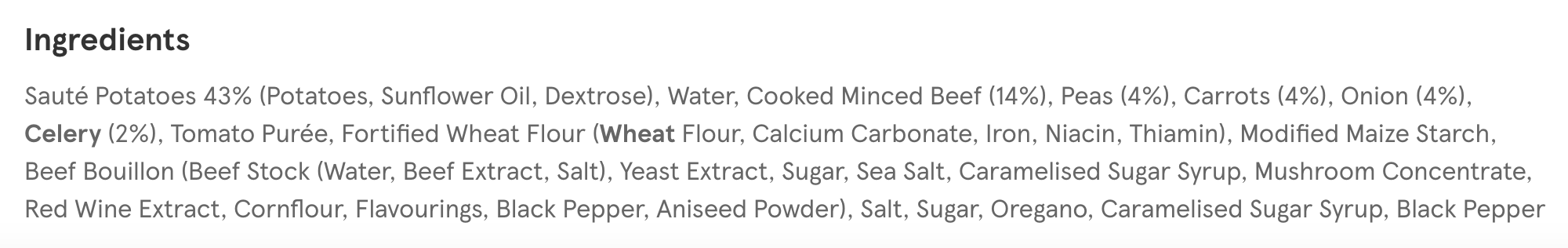
- Focus on choosing carbohydrates with a lower glycemic impact, such as whole grains and cereals. A more restrictive carbohydrate diet can be considered, tailored individually and supervised by a specialized professional.
- Maximum consumption of 5 to 10% of calories from sucrose is allowed, provided that an overall balanced diet is maintained.
- Adequate fibre intake—at least 20g of fibre for every 1000 kcal in the diet.
- Pay attention to Vitamin C intake since its absorption is impaired in diabetes.
- The best dietary pattern: Mediterranean Diet—a diet based on vegetables, seeds, low intake of red and processed meats, and rich in antioxidants and phytochemicals.
- If obesity is present, a calorie-deficit diet is recommended to reduce body fat, aiming to lower low-grade inflammation that worsens diabetes outcomes.
- Control fat intake, as an increase in intramuscular fat raises insulin resistance.
What is the glycemic load of a meal? And why is it important for diabetes treatment?
Glycemic load refers to the amount of glucose (sugar) in your blood after consuming a meal. For example, white bread has a high glycemic load, meaning it will quickly raise blood sugar levels. On the other hand, foods that take longer to digest, such as those rich in protein and fats, have a lower glycemic load.
Understanding which foods have a low glycemic load helps control blood sugar levels in patients with diabetes, which is essential for preserving pancreatic health and avoiding the complications of uncontrolled diabetes mentioned earlier.
And what about fibre? Do you know how fibre works in controlling blood sugar?
Fibre plays several roles in blood sugar control. Soluble fibres (found in oats, apples, carrots, and beans) help regulate glucose absorption by forming a gel that slows digestion. This gradual and slowed absorption of glucose prevents spikes in blood sugar levels.
Insoluble fibres (found in whole grains, nuts, and vegetables) do not dissolve in water and therefore increase stool bulk, leading to less sugar being absorbed.
Additionally, these fibres serve as food for our gut bacteria, which are known to improve insulin sensitivity and help in better diabetes management.
Moreover, fibre plays a significant role in appetite control, helping to regulate calorie intake throughout the day.
Why is the Mediterranean diet associated with the treatment of diabetes?
The Mediterranean diet, which is plant-based and includes seeds, vegetables, and nuts, is rich in fibre, low glycemic index foods, and antioxidants. This diet helps treat type 2 diabetes on multiple fronts, improving insulin sensitivity and reducing inflammation and oxidative stress, which are common in diabetes.
Is it possible to reverse type 2 diabetes?
Yes, it is possible in many cases, especially when detected early and pancreatic function is still preserved. Reversing diabetes means normalizing blood sugar levels without the need for medication.
Factors that facilitate this reversal include significant weight loss with a reduction in visceral fat, lifestyle changes involving healthy eating habits (rich in vegetables, whole grains, lean proteins, and low in sugars and refined carbohydrates), and regular physical exercise.
However, it’s important to understand that there is no cure, so the risk of re-developing diabetes remains. This is why long-term lifestyle changes and continuous monitoring are essential.
Regarding type 1 diabetes, which is an autoimmune disease, the same chances of reversal do not apply.
How a nutritionist help you reverse type 2 diabetes?
Through consultations with a registered dietitian or nutritionist, your complete health history will be combined with your dietary history to create a personalised nutritional treatment plan that meets all your individual nutritional needs. When necessary, they also prescribe nutritional supplements to support the success of your treatment.
Our clinic of diabetes dietitian and nutritionist offers a significant advantage in supporting lifestyle changes. We understand that habit changes are challenging and require ongoing support. We provide an app that allows daily contact with your nutritionist, where you can ask questions, receive tips to overcome daily challenges, get encouragement, and have your meal plans adjusted whenever needed.